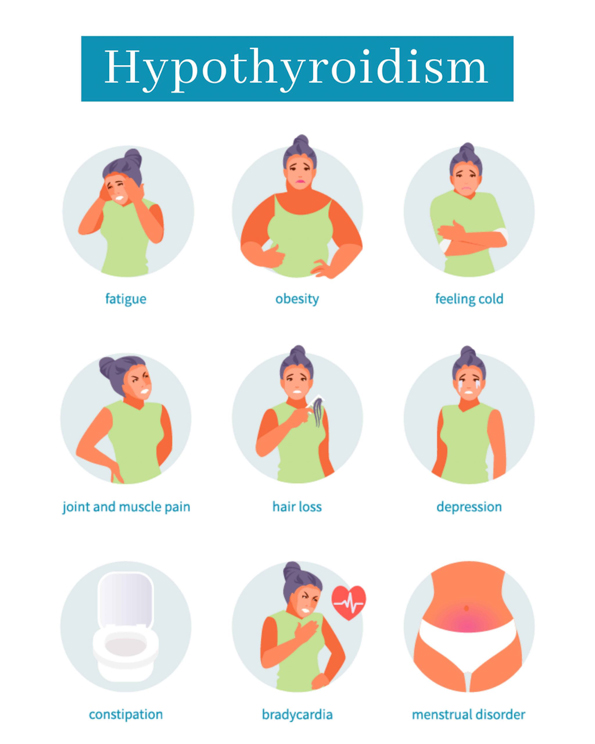
Hypothyroidism occurs when the thyroid gland produces an inadequate amount of thyroid hormone. This causes a “slow down” of body metabolism leading to fatigue, drowsiness, forgetfulness, difficulty with learning, dry, brittle hair and nails, itchy skin, puffy face, constipation, sore muscles, weight gain, fluid retention, heavy and/or irregular menstruation, increased frequency of miscarriages and/or increased sensitivity to cold. The most common cause of hypothyroidism is autoimmune thyroiditis (Hashimoto’s thyroiditis). Other causes include damage to the pituitary gland which is responsible for producing thyroid stimulating hormone (TSH), congenital hypothyroidism (infants born with in adequate thyroid tissue), medications such as lithium, iodine, and amiodarone, and postpartum thyroiditis (hyperthyroidism after giving birth followed by several months of hypothyroidism). Radioactive iodine treatments and surgeries on the thyroid gland or the removal of thyroid can also cause hypothyroidism (AACE, n.d.).
Hypothyroidism is diagnosed by elevated serum TSH concentration noted in blood work. For women who plan to conceive, it is important to maintain their thyroid hormone levels since the imbalance can affect the development of the baby. The thyroid replacement requirements also change during pregnancy and warrant closer monitoring. It has also been found that hypothyroidism is associated with increased rate of first trimester miscarriage. Women with hypothyroidism planning for conception should work with a provider to optimize their thyroid hormone levels both pre and post conception. Increased obstetric complications have also been observed including preeclampsia, gestational hypertension, placental abruption, nonreassuring fetal heart tracing, low birth weight, preterm delivery, increased rate of c-section, postpartum hemorrhage, perinatal morbidity and mortality, and neuropsychological and cognitive impairment in the child. The treatment of choice is levothyroxine (T4) and the goal is to restore thyroid function as soon as possible. The thyroid levels are typically monitored 4-6 weeks aftermedication initiation and dose adjustments. The goal preconception serum TSH level is <2.5 mU/L (Ross, 2021).
For more information or to schedule a consultation with one of our physicians, please contact us at 808-545-2800 or visit our website at https://www.ivfcenterhawaii.com
References
- American Association of Clinical Endocrinology. (n.d.). What is hypothyroidism? https://www.aace.com/disease-and-conditions/thyroid/what-hypothyroidism
- Ross, D. (2021). Hypothyroidism during pregnancy: Clinical manifestations, diagnosis, and treatment. UpToDate. https://www.uptodate.com/contents/hypothyroidism-during-pregnancy-clinical-manifestations-diagnosis-and-treatment