In Vitro Fertilization
The Fertility Institute of Hawaii has some of the world’s leading experts on In Vitro Fertilization with over 30 years of experience treating infertile couples. The doctors (Dr. John Frattarelli, Dr. Anatte Karmon, and Dr. Emily Goulet) are the most experienced IVF providers in Hawaii having personally overseen more than 35,000 fertility treatment cycles that resulted in more than 15,000 babies born.
Certified as a High-Complexity Clinical Laboratory Director (HCLD), Dr. John Frattarelli, HCLD is one of only a few physicians nationally and the only physician in Hawaii who also is qualified to serve as Laboratory Director for the IVF Laboratory. This allows him to provide unique oversight for all Clinical and Laboratory aspects of the IVF practice. This unique oversight of the entire program contributes to the tremendously high pregnancy rates that the Fertility Institute of Hawaii is able to achieve.
 The IVF laboratory of the Fertility Institute of Hawaii has been awarded an accreditation by the Commission on Laboratory Accreditation of the College of American Pathologists (CAP), based on the results of an on-site inspection. The accreditation indicates that our laboratory is one of an exclusive group of reproductive laboratories around the country that have met the highest standards of excellence. Our laboratory facility undergoes and passes a yearly CAP evaluation.
The IVF laboratory of the Fertility Institute of Hawaii has been awarded an accreditation by the Commission on Laboratory Accreditation of the College of American Pathologists (CAP), based on the results of an on-site inspection. The accreditation indicates that our laboratory is one of an exclusive group of reproductive laboratories around the country that have met the highest standards of excellence. Our laboratory facility undergoes and passes a yearly CAP evaluation.
The CAP Laboratory Accreditation Program is an internationally recognized program that helps laboratories achieve the highest standards of excellence to positively impact patient care. The goal of the CAP Laboratory Accreditation Program is to improve patient safety by advancing the quality of pathology and laboratory services through education, standard setting, and ensuring laboratories meet or exceed regulatory requirements. CAP inspectors also examine the entire staff’s qualifications, the laboratory’s equipment, facilities, safety program and record, as well as the overall management of the laboratory.
The Fertility Institute of Hawaii has offices on Oahu in Honolulu and on the windward side in Kailua. The providers also see patients in Maui and on the Big Island in Hilo and Kona. The Fertility Institute of Hawaii’s IVF program has consistently had superior pregnancy rates that ranked as one of the best in the world.
Related Videos:
Frequently Asked Questions
IVF Presentation
What is involved with In Vitro Fertilization?
IVF is a procedure designed to enhance the likelihood of conception in couples for whom other fertility therapies have been unsuccessful or are not possible. It is a complex process and involves multiple steps resulting in the insemination and fertilization of oocytes (eggs) in our laboratory. The embryos created in this process are then placed into the uterus for potential implantation.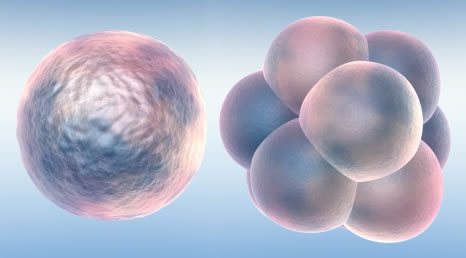
In Vitro Fertilization is commonly referred to as IVF. IVF is the process of fertilization by manually combining an egg and sperm in a laboratory dish. When the IVF procedure is successful, the process is combined with a procedure known as embryo transfer, which is used to physically place the embryo in the uterus.
The IVF process can be broken down into five steps which include the following:
- Step 1 • Initiation of the IVF Cycle. During the first phase of an IVF cycle, patients are typically treated with medications that may include oral contraceptives or estrogen to coordinate the start of the treatment cycle. Depending on a patient’s history and health, additional medications are sometimes administered to prepare a woman for ovarian stimulation.
- Step 2 • Ovulation Induction. Women normally produce a single mature follicle containing an egg during each menstrual cycle. This process is regulated by a naturally occurring hormone called follicle-stimulating hormone (FSH). During the ovulation induction phase of the IVF cycle, the woman is treated with an injectable form of FSH that is identical to naturally produced FSH. The FSH stimulates her ovaries to produce multiple follicles containing eggs to grow and mature. Multiple follicle development is advantageous because a significant percentage of the eggs a woman produces are abnormal. The percentage of abnormal eggs increases with age. At this stage of treatment, other hormones (GnRH analogs) are used to prevent the ovary from releasing an egg too soon. Your provider will monitor this process with an ultrasound and blood work over the course of treatment, usually lasting 9 to 11 days.
- Step 3 • Oocyte Retrieval. Once the follicles containing the eggs have reached an appropriate size, a hormone (hCG analog) injection is used to mature the eggs. Thirty-six hours after the injection, the eggs are removed from the ovaries in a minor surgical procedure called a ‘vaginal oocyte retrieval’. Anesthesia is administered to ensure patient comfort during this process. Guided by an ultrasound probe inserted into the vagina, your provider will direct a needle into the follicles of the ovary to retrieve the eggs. The procedure takes anywhere from 10 to 30 minutes. Most women are able to return home an hour or so after the retrieval. On the next day, progesterone is started to prepare the uterus for implantation of the embryo.
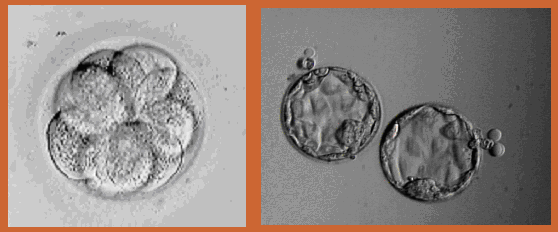
- Step 4 • Oocyte Fertilization and Embryo Development. Once removed from the follicles, the eggs are examined by an embryologist and prepared and placed in an incubator. The eggs are then inseminated. The next day, the eggs are checked to see if they have been fertilized. The fertilized eggs, now called embryos, are then placed in a special medium to promote their growth before they are transferred to the uterus. Embryos are typically allowed to grow in the laboratory for 3 to 6 days before being cryopreserved or transferred into the uterus.
- Step 5 • Embryo Cryopreservation and Embryo Transfer. Embryos that have been cultured in the laboratory can be placed into a woman’s uterus using a catheter, which is inserted through the cervix or cryopreserved for future transfer. During the embryo transfer, your provider will use an ultrasound to help guide the catheter to ensure appropriate placement. After the embryo transfer, progesterone is continued. About 10 days after embryo transfer a pregnancy test is done. If a pregnancy is confirmed, progesterone is continued for an additional four to six weeks until the placenta begins to produce enough progesterone to support the pregnancy on its own.
Ovarian Follicle Development
In a normal menstrual cycle, only one egg/oocyte each month develops and matures. The egg matures with a fluid filled structure on the ovary called a “follicle” which can be seen on ultrasound. In an Assisted Reproductive Technology (ART) cycle, ovulation induction medications (typically daily self-administered injections) are used to stimulate the ovaries so that multiple follicles (eggs) will develop.Depending on your stimulation protocol, you may begin your first medication in the menstrual cycle preceding the IVF cycle. Then, after your next period, the ovulation induction hormones are begun. Exact instructions regarding their use will be given to you at that time by the staff. These medications will be used for approximately 8 to 12 days, depending upon how your ovaries respond. These medications and their use will be explained in detail before each cycle.
When the majority of follicles have reached a mature size (17 to 20 mm), another medication, human chorionic gonadotropin (hCG), will be given by injection. The hCG must be given at the appropriate time of follicle development to prepare the egg for removal from the body.
Monitoring of Ovarian Follicular Development
Beginning around cycle day 3, we will draw blood samples every 1 to 3 days to monitor the hormones levels in your blood. These blood tests will be used to determine if the levels are in the range that we would expect prior to ovulation.Ultrasound monitoring of the ovaries will also be used to follow follicular growth. The ultrasound machine works by sending out sound wave signals which reflect off different structures in the pelvis and give an image of follicles growing on each ovary. When indicated by your hormone levels, ultrasounds will be performed daily as well.
Because ultrasounds are performed using a vaginal probe, you do not have to fill your bladder for this procedure. There have been no harmful effects to developing oocytes or early pregnancy from ultrasound. Monitoring and daily decisions about your care are made by your provider.
Day of Trigger Injection
When ultrasound and blood estradiol levels indicate that the follicles are maturing, you will be instructed to give the trigger injection in the evening. Depending on your individualized IVF protocol, your injection may consist of HCG, Lupron, or a combination of both. You will be told the specific day and time to give your injection. The egg retrieval is usually performed 34-37 hours after the trigger injection is given. We ask that the male partner refrain from sexual intercourse from the time of trigger until after the egg recovery, in order to obtain the best sperm sample possible.The morning after your hCG injection you will receive final instructions for egg recovery and final medications.
Vaginal Ooocyte (Egg) Retrieval (VOR)
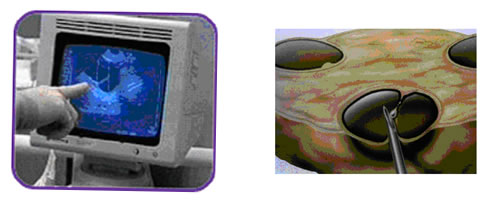 The majority of IVF patients have a sonographic egg recovery performed. This procedure uses ultrasound guidance to retrieve oocytes from your ovaries. The physician places the ultrasound probe into the vagina and guides the aspirating needle through the vagina into follicles on each ovary. Fluid is aspirated from the follicles and transferred to the embryologist, who will identify the eggs under the microscope.
The majority of IVF patients have a sonographic egg recovery performed. This procedure uses ultrasound guidance to retrieve oocytes from your ovaries. The physician places the ultrasound probe into the vagina and guides the aspirating needle through the vagina into follicles on each ovary. Fluid is aspirated from the follicles and transferred to the embryologist, who will identify the eggs under the microscope.
Eggs are cultured and fertilized in the Embryology Laboratory.
Sperm (Semen) Collection
During or immediately following the egg recovery, the male partner will need to give a sperm sample. A private room is provided for discrete semen collection. Patients who need to use donor sperm will be given instructions on ordering donor sperm at the time of the initial screening appointment.
Culture and Fertilization of the Oocyte(s)
 Once the eggs are retrieved, they will be placed in special fluid media for approximately 6 to 12 hours. The semen specimen will be prepared to isolate the best sperm for insemination, then placed with the eggs and incubated overnight. Intracytoplasmic sperm injection (ICSI) may be performed instead for any sperm abnormalities detected.
Once the eggs are retrieved, they will be placed in special fluid media for approximately 6 to 12 hours. The semen specimen will be prepared to isolate the best sperm for insemination, then placed with the eggs and incubated overnight. Intracytoplasmic sperm injection (ICSI) may be performed instead for any sperm abnormalities detected.
The eggs will then be examined for signs of fertilization, and normally fertilized eggs will be placed into a special growth medium. Cutting-edge technologies such as the EmbryoScope incubator may be used to help guide embryo selection and improve success rates. Normally developing embryo(s) will be transferred back into your uterus three to six days after egg recovery, depending on the number and quality of the embryos as they develop in our laboratory.
Not all follicles aspirated can be expected to yield an oocyte. Moreover, all kinds of oocytes can be recovered: mature, immature, and post-mature or degenerate. You will be notified about the number of eggs that have fertilized the day after egg retrieval. Detailed information about the developing embryos will be available at the time of embryo transfer, at which point you will have an opportunity to discuss these results with your provider. Some patients require special therapy such as assisted hatching to enhance implantation of the embryos. These therapeutic options will be discussed in detail with you at your appointments.
This is the return of the embryos that have developed in our laboratory into your uterus. You will lie on an examination table as if you were going to have a Pap smear. There will be no anesthetic required. A very fine soft catheter is placed through the cervix into the uterine cavity under ultrasound observation, and the embryos are transferred inside the uterus through the cervix. Your partner or a friend may be with you during the transfer and during the 15 minute rest period.
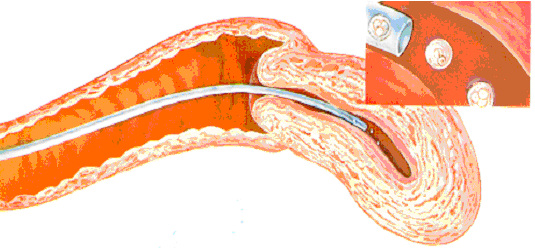
The practice of transferring multiple embryos to a woman’s uterus increases her chance for a pregnancy, but also raises the odds of having a multiple birth. The rate of multiple births for ART is higher than that of the normal population. Most of these are twin pregnancies; however, if more than two embryos are transferred, the risk of higher order multiple pregnancies (e.g. triplets) becomes a concern. Multiple pregnancies have increased risks for both mother and babies, particularly preterm delivery.
You will speak to your provider about your chances of pregnancy and risk for multiple pregnancy. Together, you can determine the appropriate number of embryos to transfer (usually one to three) depending on your personal medical situation.
Embryo Cryopreservation(s)
Many patients will have embryo cryopreservation with a subsequent frozen-thawed embryo transfer rather than an embryo transfer immediately after the egg retrieval. Your provider will discuss this option with you in detail during your IVF cycle. Depending on your personal medical situation and the quality and number of embryos, you will have the option of cryopreserving (freezing) the remaining embryos for thawing and replacement at a later time. You can learn more about cryopreservation in the fertility preservation section of our site.
Follow-up Blood Tests and Obstetrical Appointment
You will need to have a pregnancy test 10-12 days after the embryo transfer. We recommend the pregnancy test and first two obstetric ultrasounds (if applicable) be done with our practice. We are also anxious to know the outcome of your cycle, and are better able to offer medical and emotional support if we are informed right away.Once pregnancy has been confirmed to be doing well with the ultrasound and bloodwork, we will discharge you to your OB/GYN to continue obstetrical care or, if you do not have one, we can provide names of excellent general obstetrician/gynecologists in your area.
Unfortunately not all ART cycles result in pregnancies, you are encouraged to arrange a follow-up appointment with your provider. The purpose of this visit would be to summarize your cycle, answer questions, and discuss future plans, such as future ART cycles, other infertility options or non-medical family building options.
Theoretical Concerns & Potential for Success
Unfortunately, neither conception nor a successful outcome of pregnancy is guaranteed by the IVF-ET procedure. There are many reasons why pregnancy may not occur with the IVF-ET procedure. In fact, there are complex and largely unknown factors that limit pregnancy rates following assisted reproductive techniques. Some of the known reasons for failure may include, but are not limited to:
-
- There may be a failure to recover an egg because:
- follicles that contain mature eggs may not develop in the treatment cycle
- ovulation has occurred before time of egg recovery
- one or more eggs cannot be recovered
- pre-existing pelvic scarring and/or technical difficulties prevent safe egg recovery
- The eggs that are recovered may not be normal.
- There may be insufficient semen to attempt fertilization of the recovered eggs because the man is unable to produce a semen specimen, because the specimen contains an insufficient number of sperm to attempt fertilization, because the laboratory is unable to adequately process the specimen provided, or because the option to use a donor sperm as a “backup” was declined.
- Fertilization of the eggs to form embryos may fail even when the egg(s) and sperm are normal.
- The embryos may not develop normally or may not develop at all. Embryos that display any abnormal development will not be transferred.
- Embryo transfer into the uterus may be difficult/impossible, or implantation(s) may not occur after transfer, or the embryo(s) may not grow or develop normally after implantation.
- Any step in the IVF-ET process may be complicated by unforeseen events, such as hazardous or catastrophic weather, equipment failure, laboratory conditions, infection, human error and the like.
- There may be a failure to recover an egg because:

